- July 11, 2023
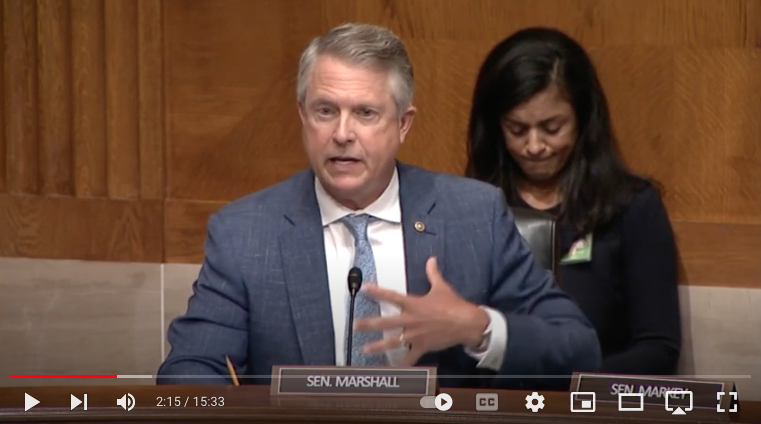
Senator Marshall Leads Hearing on Superbugs Unraveling Modern Medicine
Washington, D.C. – Today, U.S. Senator Roger Marshall, M.D., chaired the Health, Education, Labor, and Pensions (HELP) Subcommittee hearing, Superbugs: The Impact of Antimicrobial Resistance on Modern Medicine. As Ranking Member of the Subcommittee, Senator Marshall led the discussion on antimicrobial resistance (AMR) unraveling medical breakthroughs in cancer treatment and other life-threatening illnesses. The witnesses testifying represented physicians, manufacturers, patients, and researchers across the country. Notably, the panel included native Kansan Michael Apley, a clinical researcher from Kansas State University and former member of the Presidential Advisory Council on Combating Antibiotic-Resistant Bacteria.
You may click HERE or on the image above to listen to Senator Marshall’s full opening remarks.
Highlights from Senator Marshall’s opening remarks include:
“This is why I came to Congress was to fix problems like this. And I’ll tell you why this is near and dear to my heart. Certainly, the second year medical student tried to understand bacteria and yeast infections and fungus, but the story that I remember is showing up for my OB-GYN residency program. The story that haunted everybody was a young lady that had a C-Section, and had died maybe three months before I got there. And she died from a resistant bacteria, from sepsis, a complication from a C-Section. And very few days, or weeks went by that we didn’t talk or they didn’t talk about that case.”
“3 million Americans this year will get some type of an antimicrobial resistant superbugs this year. 100 Americans will die today, 100 will die tomorrow, and every day this year from some type of a resistant bug.”
“And I see the need for this rising as diabetes and obesity overwhelm our society. Those are setups for more resistant organisms. And again, in my field of obstetrics, our C-Section rates are going up for the same reasons. And we’re going to have more infections and more resistant bugs and then of course, sexually transmitted diseases.”
“When we develop these types of antibiotics, we’re hopefully only going to use them each a handful of times… We have many professional friends and colleagues who have asked me to have this patient centered hearing. So I’m so proud of the all star group of witnesses we have. I know it’s going to be a great, great hearing. And again, I want to emphasize- thank you to your staff as well, Chairman and the committee’s staff working together to bring this to light. This is an issue that this committee can literally make a difference today.”
Commonly referred to as a silent epidemic, AMR is increasing the risk of death due to unmanageable infections, and in 2019, it led to 4.95 million deaths worldwide, making it the third leading cause of death after cardiovascular disease and cancer. It impacts more than 2.8 million Americans each year and kills more than 35,000 people annually. The commercial marketplace for antibiotics in the U.S. is at serious risk of collapsing due to ongoing reimbursement challenges and supply chain shortages. In his opening remarks, discussed these industry challenges and shared examples from his nearly 30-year career as an OBYN treating various bacterial, viral, and fungal infections daily. He also commended the livestock and agriculture industry for their stewardship of antibiotic use.
Senator Marshall advanced many AMR policies since first joining Congress. The Infectious Diseases Society of America (IDSA), a national medical association representing health care professionals specializing in infectious diseases, recently recognized Senator Marshall for his leadership and presented him with the 2023 Legislative Impact Award. Specifically, the organization commended him for spearheading an annual bipartisan effort in support of federal investments to combat AMR.
Highlights from Senator Marshall’s questioning include:
Senator Marshall: Most of your patients you see are probably people that survive organ transplants, that maybe they’ve taken cancer therapy recently, and then we lose them to an infection. What would the message of hope be that you give to a cystic fibrosis patient?
Dr. Boucher, Dean and Professor of Medicine, Tufts University School of Medicine: What we physicians and all clinicians need is tools in our toolbox, right? We need ways to prevent infection. And we need drugs to treat those infections, which still happens. So it’s not just one, as was pointed out earlier, we need a pipeline that is robust and renewable, because we know resistance will march on.
Senator Marshall: What’s it like to watch your patients die because you don’t have the right antibiotic? You know, it starts off as a kidney infection, starts off with pneumonia. What’s it like to watch them die and not have the antibiotic that you need?
Dr. Boucher, Dean and Professor of Medicine, Tufts University School of Medicine: I’ll just start by saying I chose the profession of infectious diseases 30 years ago to cure patients, right? Antibiotics, as Senator Markey said at the open, are curative, life saving drugs. So I came into this field to cure people of infections and send them home to live their lives, to enjoy the transplant, that precious gift that they get.
So coming to the point where I’ve had the sad duty to sit with a lady who lived through rounds of chemotherapy for her leukemia, who had an infection for which we had no therapy, and to watch her go from sitting in the chair, to sicker and sicker and dead in a number of days, is beyond heartbreaking.
Senator Marshall: Speak a little bit about agriculture protein production. What we’ve done to decrease the use of antibiotics and to address these issues and specifically, talk a little bit about how the 2017 law has impacted your world.
Dr. Apley, Professor, College of Veterinary Medicine at Kansas State University: If you go back to 2017 and look at the FDA sales data for antibiotics following that, and 2017 was the start of the transition to all medically important antibiotics used in feed to the veterinary feed directive and any Euston water to under veterinary control. And the next year we saw, for example, tetracycline use dropped by around a third, as the veterinarians took control of that and had discussions with their clients based on the stewardship principles. You know, the last time a new antibiotic group was approved that we use in food animals was 1978, that a new group was approved. So we are using tried and true older compound groups, we get new members of them.